DXA Tech QRG: Algorithms Used in Bone Densitometry
Radiologic technologists, specifically DXA operators, must understand DXA scan analysis and some of the algorithms used in bone densitometry. This article offers greater insight into what goes on behind the scenes in a DXA machine. There are also some useful tips to make your scanning more accurate.
Computation of Soft Tissue Density
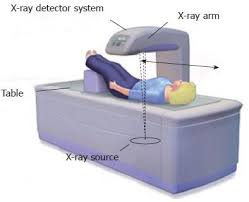
DXA scans play a critical role in the diagnosis and treatment of osteoporosis. The underlying principle of DXA scan analysis is that X-Rays produced by a DXA machine are detected by sensors after they pass through the patient’s body. The intensity of the X-Rays is decreased (attenuated) when it passes through the tissues of the body. The extent to which the X-Rays are attenuated is determined by the intensity of the beam. It is also influenced by the thickness and density of the patient’s tissues. For each intensity level of the X-Ray beam, every tissue has a unique attenuation profile. This can be expressed as an attenuation coefficient. However, in the human body, soft tissue surrounds bones and the model is not straightforward. Therefore, in DXA scans, there is a need to distinguish bone from surrounding tissue in terms of density.
In DXA scan analysis, the passing of two energies of photons (one high and one low) through the body is measured. This method involves dividing the body into two parts – bone and soft tissue. Bone contains a mineral component made up of high atomic number elements such as calcium and phosphorus. Soft tissue, on the other hand, is a mix of skin, fat, muscle, and water with a density that is lower than bone. Therefore, the same energy is attenuated to a different degree by the two components and each has a specific attenuation coefficient. When there are two X-Ray energies, such as with DXA, the attenuation coefficient of each type of tissue can be applied to two equations, one for each energy peak. Subtracting the attenuation of low-energy photons from the attenuation of high-energy photons gives the area density of bone.
Bone Edge Detection
It is important for the bone edges to be correctly detected during DXA scan analysis for bone and soft tissue to be correctly separated. Incorrect edge detection can lead to falsely high or low BMD. For example, mapping the edge inside the spine leads to a falsely high BMD because it decreases the area and includes tissue with high mineral content. On the other hand, detection of edges outside the hip or spine leads to a false decrease in BMD because it increases the area and includes more low-density tissue.
Every DXA device manufacturer has a unique bone edge detection algorithm that enables separation of soft tissue and bone. Technologists should keep in mind that if DXA scan analysis algorithms designed for adults are used in the pediatric population, they will fail because of the lower body weight and lower BMD of the pediatric patient. In other words, the DXA device will be unable to correctly identify where bone finishes and soft tissue begins.
It is possible for the DXA technologist to see bone edge detection failure and correct it. Machine mapped bone edges should be verified by the technologist and corrected if necessary. Manufacturers of DXA machines are working on improving DXA scan analysis bone edge detection as well. Hologic has introduced special software for imaging spines with low density to address edge detection issues. This analysis mode can be selected by the operator when the patient is known to have low bone density.
Bone Edge Detection in Obese and Thin Patients
The limitations of DXA scan analysis technology are tested by patients who are either extremely thin or extremely obese and/or patients with very low bone mass. In such patients, bone edge detection problems manifest as a moth-eaten or mottled appearance of the image. The DXA technologist should use the fastest scan speed for thin patients and the slowest scan speed for obese patients. There are certain clues that indicate to the DXA technologist that bone edge detection is faulty. For example, an inordinately large Ward’s area or extremely small trochanter are indications of poor bone edge detection in hip scans. If the patient’s hip is deemed unsuitable for DXA scanning due to poor bone edge detection, consideration should be given to the non-dominant forearm as an alternative site.
BMC, BA, and BMD
A DXA scan analysis report has three key values:
- Bone mineral content (BMC) in grams. This indicates the amount of mineral mass (hydroxyapatite) in bone. Note that BMC does not include the organic content of bone (collagen and marrow).
- Bone area (BA) in square centimeters. This indicates the area of bone included in the scan.
- Bone mineral density (BMD) in grams/cm2. This indicates the mineral mass per unit of imaged area. This is the area bone mineral density (aBMD). True volume density can be measured by quantitative CT. Therefore, DXA measures aBMD (grams/cm2) which is the BMC in grams divided by the BA in cm2.
The difference between area BMD and volume BMD can be illustrated by the following example. Let’s say two patients have the same bone density when measured by quantitative CT. When the same two patients undergo bone density measurement by DXA scan analysis, the taller of the two patients will have a higher BMD. This is because the areal BMD measured by DXA does not differentiate between low-density large bones and high-density small bones. Therefore, DXA overestimates BMD in taller/larger patients and underestimates BMD in shorter/smaller patients.
DXA Scan Analysis
DXA machines measure bone density for each pixel as the X-Ray source and detector assembly moves over the scanned region. This generates a pixel-by-pixel profile of bone density after multiple linear passes over the scan field. This profile then undergoes DXA scan analysis by the software in the device using an algorithm for edge detection that identifies the border between bone and surrounding tissues in the scan area. The machine then calculates the average density across the scanned profile. The bone area (BA) is calculated by adding up bone-containing pixels. The average density in g/cm2 multiplied by the bone area (BA) in cm2 gives the bone mineral content (BMC) in grams.
Further Reading
Advice for Patients with Osteopenia
DXA Osteoporosis Test: Does My Patient Need It?
DXA Operator Continuing Education
To complete your CEUs, please visit this page and purchase one of our online e-courses and tests. All courses on our website offer category A credits which are good for your ARRT® CE requirements and are accepted by NMTCB, ARDMS, SDMS, every US state and territory, Canadian province, and all other Radiologic Technologist, Nuclear Medicine, and Ultrasound Technologist registries in North America, for both full and limited permit technologists, guaranteed. We give you the flexibility to choose a course with the number and type of credits you need.
Get more information about continuing education for radiologic technologists here.