Fracture Risk Assessment Tool: An Overview for X-ray Techs
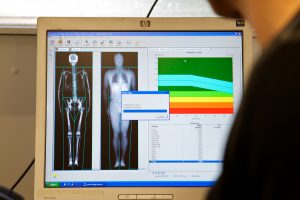
The gold standard in diagnostic testing for osteoporosis and fracture risk is bone mineral density (BMD) measurement. However, it is neither cost-effective nor practical to perform BMD testing in every individual and use this as a fracture risk assessment tool. The majority of people are not at risk of bone disease. Thus, BMD testing is recommended only in populations that are known to be at high risk, such as women over the age of 65. What are some of the other fracture risk assessment tools available to healthcare providers?
As stated, indiscriminate BMD testing does not make sense, either medically or economically. It is, therefore, important to identify individuals who are at risk of bone disease and are most likely to benefit from BMD measurement. This must be accomplished with an accurate fracture risk assessment tool.
Who is at High Risk of Fractures?
Besides women over 65, some men and younger women may have one or more risk factors that qualify them for BMD testing. For instance, it is important to identify the subset of people who, irrespective of age or gender, have had a prior fragility fracture. They are candidates to undergo testing with a fracture risk assessment tool. It is also important to identify people who have diseases that increase fracture risk. It should be noted that certain risk factors are directly associated with BMD while others, such as fall risk, are independent of BMD.
There are certain risk factors, such as age, gender, and prior spine fracture, which are universally accepted clinical recommendations for BMD testing. Because advancing age is a major risk factor for fractures, it has been suggested that all Caucasian women above the age of 65 years undergo BMD testing. In addition, younger (premenopausal) women with one or more risk factors should also be tested with BMD or some other fracture risk assessment tool. Interestingly, the presence of risk factors not only determines an individual’s candidacy for diagnostic testing, but also directs treatment. For example, treatment is recommended in people with a history of spine fracture due to minimal trauma even if they do not have low bone mineral density.
What is the Ideal Fracture Risk Assessment Tool?
There is currently no universal analysis tool that can be used for screening to clinically predict fracture risk. Ideally, a fracture risk assessment tool should be based on factors that can be easily measured clinically, such as height, weight, prior history of fractures, and family history of bone disease. The goal of risk factor analysis is to perform individualized diagnosis for every person regardless of age, gender, or ethnicity. To save time for busy physicians, non-physician healthcare personnel should be able to administer and interpret the fracture risk assessment tool, for instance, by obtaining answers to a short questionnaire that helps identify at-risk individuals. Several clinical risk assessment tools are under development; however, all have some limitations or problems that need to be addressed.
Osteoporosis Risk Assessment Instrument
ORAI (Osteoporosis Risk Assessment Instrument) is a fracture risk assessment tool that takes into account an individual’s age, body weight, and use of estrogen. This tool can identify 93 percent of people who have a low bone mineral density. However, it is only 39 percent specific. In other words, 61 percent of people identified by this tool do not, in fact, have a low BMD.
Simple Calculated Osteoporosis Risk Estimation
SCORE (Simple Calculated Osteoporosis Risk Estimation) is a fracture risk assessment tool that takes into account six factors – age, body weight, race, use of estrogen, personal fracture history, and rheumatoid arthritis. This tool has 91 percent sensitivity and 40 percent specificity, similar to the ORAI tool.
Osteoporosis Self-Assessment Tool
OST (Osteoporosis Self-Assessment Tool) takes into account two risk factors, the individual’s age and body weight. The results of this tool reveal 92 percent sensitivity and 46 percent specificity.

Dubbo Osteoporosis Epidemiology Study
A fracture risk assessment tool and scoring system was developed based on the Dubbo Osteoporosis Epidemiology Study. This system took into account the individual’s age, weight, and prior history of fractures. Although this tool is good at predicting low BMD, it has been found to be less accurate in predicting fractures.
Self-Administered Checklist
Clinicians can use any fracture risk assessment tool to identify the subset of patients who warrant further testing and who would benefit from BMD measurement. In addition, the National Osteoporosis Foundation has developed a checklist for every individual to assess their own risk of bone disease. This self-assessment checklist allows individuals to become aware of risk factors and to discuss concerns about bone health with a medical professional. While the foundation has not developed a specific scoring system for medical professionals to use, it has issued practice guidelines that take into account age, weight, smoking status, personal history of fractures, and family history of fractures.
Limitations of Existing Fracture Risk Assessment Tools
The inherent problems and limitations associated with existing fracture risk assessment tools have prevented their widespread clinical use. One issue is that there is limited medical knowledge about which risk factors should prompt further evaluation. Epidemiologic studies on large populations have shown that age, gender, and ethnicity are important predictors of risk, but uncertainty remains about which of these characteristics should be included in the clinical tools used to assess risk of bone disease.
Studies that have evaluated risk factors have largely focused on Caucasian women above the age of 65, a known high-risk population. Other populations have been less well documented. Therefore, risk factors that are different between men and women, between older and younger individuals, and between people of different races are not completely understood. Known risk factors account for only 20-33 percent of differences in bone mineral density between individuals. Thus, it is evident that many risk factors remain undiscovered. This makes it difficult to apply fracture risk assessment tools.
Height Loss and Fracture Risk
One important risk factor that is indicative of potential bone disease and is not included in any of the fracture risk assessment tools is height loss. Decreased muscle strength, poor posture, and narrowing of the intervertebral disc spaces are some of the conditions that can lead to height loss and curvature of the spine. However, osteoporosis should be considered in any individual with a measurable height loss of more than 1 inch. New or progressive curvature of the spine should likewise serve as a red flag to healthcare providers because this can be indicative of osteoporosis-induced compression fractures in the vertebrae.
In addition, monitoring changes in height is a useful method of assessing whether preventive and therapeutic measures for osteoporosis have had an impact. The problem with measuring height is that people are often unsure or inaccurate in their recollection of previous measurements. Moreover, current height is frequently not measured accurately. Specialty clinics have access to tools such as kyphometers and stadiometers which measure height and spinal curvature accurately, but these tools are not widely available. The use of these devices along with a fracture risk assessment tool can improve identification of high-risk individuals.
Clinical Tools for Fracture Risk Assessment
In addition to identifying individuals who should undergo BMD testing, clinical fracture risk assessment tools are being developed to answer other questions, such as which individuals are at high risk of fractures. Once a subset of people who are at high risk of fractures is identified, preventive measures and early interventions can be instituted.
A large study called the Study of Osteoporotic Fractures has been used to develop a risk assessment tool that takes into account several risk factors that cause hip fractures in elderly Caucasian women, independent of their bone mineral density and personal fracture history. Some of the risk factors included in this tool are maternal fracture history (genetic), weight change, height loss, and exercise (lifestyle). All these risk factors have been shown to be important in identifying individuals with a high fracture risk.
A study showed that patients with BMD in the lowest third of the study population as well as BMD in the highest third of the study population both had nearly five times the risk of suffering a hip fracture, demonstrating that hip fracture risk is not related to BMD alone. This was further validated by a study that showed that women with five or more risk factors (other than low BMD) have a 17 times higher risk of hip fracture compared to women with two or less risk factors. This reiterates the need to use a fracture risk assessment tool other than BMD.
Questionnaire for Fracture Risk Analysis
Based on the most prevalent risk factors identified by the Study of Osteoporotic Fractures, a questionnaire has been developed that can be administered to patients in the clinical setting. This is an easy to use fracture risk assessment tool. Each answer on this questionnaire has been given a point value. These points are added up to calculate a total score called the FRACTURE score.
A large prospective study in Europe called EPIDOS evaluated the usefulness of this fracture risk assessment tool or questionnaire. It was found that individuals with a high FRACTURE score were at higher risk of suffering a hip fracture. It should be noted, however, that this and other risk analysis tools do not work equally well for all populations. For example, predictors of fracture in elderly nursing home residents are different from healthy community-dwelling individuals. This is because elderly residents of nursing homes not only have fragile bones but are also at a higher risk of falling.
Fall Risk and Fracture Risk
Many fragility fractures are the direct result of falling. The most important factor that has not been addressed by the currently available fracture risk assessment tools is fall risk, which is an important determinant of fracture risk. Several factors affect an individual’s fall risk, such as cognitive impairment, visual problems, balance disorders, gait difficulties, and medications.
Individuals who are found to be at high risk of falling as well as at risk of bone disease are candidates for further evaluation and intervention. Interventions in such people may consist of calcium and vitamin D supplementation, balance training and strengthening exercises to prevent falls, modifications in the living environment to remove potential hazards, adjustments in medications that potentially increase the risk of falls, and use of protective devices such as hip pads to cushion the blow should a fall take place.
Eyesight and Fracture Risk
Many older individuals do not get regular eye exams. Thus, poor vision is a critical factor that affects fall risk in the elderly, even those who wear eyeglasses. High-tech balance and gait tests are available but these are not in widespread clinical use to assess fall risk. Instead, physicians tend to rely on the patient’s history of prior falls and fear of falls as well as objective tests such as functional reach and performance-oriented mobility assessment. Every patient with a prior fall should be evaluated to determine the cause, especially patients who suffered a fall that led to a fracture. Individuals who sustain a fracture due to minimal trauma should be investigated with BMD measurement or some other fracture risk assessment tool to determine their risk of bone disease.
Continuing Education for X-ray Techs
We have a range of online courses for category-A CE credits good for the ARRT® and other national and state registries. To earn credits and brush up your knowledge on bone imaging, purchase our 23-credit course on radiographic bone densitometry. We have a variety of e-courses on mammography, fluoroscopy, radiation safety and ethics. You have the flexibility to choose the type of course and number of CEUs according to your needs.
Here is more information about ce credits for x ray techs.