Osteoporosis Fracture Risk: Tips to Recognize High-Risk Patients

Osteoporosis is characterized by low bone mass and increased risk of fractures. The disease is particularly dangerous because it is often “silent.” There are no signs and symptoms while the bone loss occurs in the background. In fact, the condition is typically diagnosed when a significant medical event such as a fragility fracture occurs. Sometimes, even fractures are not recognized clinically (2 out of 3 vertebral fractures are asymptomatic). X-ray techs and DXA operators are in a unique position to recognize osteoporosis fracture risk.
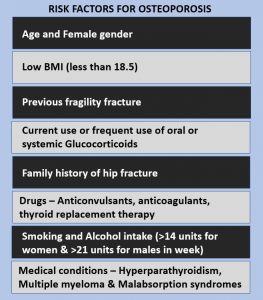
Risk Factors for Osteoporosis-Related Fractures
Osteoporosis is a common metabolic disease that affects up to 40 percent of postmenopausal women. In addition to low bone mineral density, the National Osteoporosis Foundation has outlined the following major risk factors for osteoporosis fractures:
- Personal history of fragility fracture
- Family history of fragility fracture in a first-degree relative (parent, sibling, or child)
- Smoking
- Low body weight
- Use of steroid medications
DXA Scanning, T-score, and Osteoporosis Fracture Risk
Bone mineral density measurement with dual-energy X-ray absorptiometry (DXA or DEXA) is the gold standard in the diagnosis of osteoporosis and increased fracture risk. A diagnosis is made based on DXA results (T-score) and the World Health Organizations’s definition of osteoporosis. However, the DXA result should not be used as the sole predictor of osteoporosis fracture risk. Interestingly, many patients who sustain fragility fractures have a T-score in the normal range. Fracture risk assessment tools such as FRAX take into account several clinical factors associated with an increased risk of fragility fractures. For example, age has a significant influence on osteoporosis fracture risk. In women with a normal T-score, the risk of hip fracture is 5 times higher at age 80 compared to age 50.
Identifying Patients with High Osteoporosis Fracture Risk
DXA operators should keep the following factors in mind to identify osteoporosis fracture risk in patients with normal DXA results (T-score more than -1):
Diet
Patients with a diet low in calicum and vitamin D are at increased risk of low bone mass and fragility fractures.
Lactose Intolerance
Patients with this condition have difficulty digesting diary foods which are a rich source of calcium, putting them at risk of low bone density.
Stature
Patients with small bones and low body weight are at increased risk of osteoporosis fractures.
Literacy and Language Barrier
Patients who cannot read and write and people who do not speak English fluently may have trouble reading food labels and/or understanding doctors’ instructions.
Culture
Some cultures require the whole body to remain covered (for example, Muslims). This limits exposure to sunlight which is the main source of vitamin D. Patients who remain covered all the time may need supplements for bone health.
Location
People living at northern latitudes have limited sunlight hours and may need vitamin D supplementation.
Economic Status
Patients with limited finances may not be able to afford a healthy diet or make time for exercise.
Fall Risk
Patients who are at increased risk of falling may be at higher osteoporosis fracture risk despite a normal T-score. Fall risk can be amplified by poor eyesight, medications that cause dizziness as a side effect, and living conditions.
Ethnicity and Osteoporosis Fracture Risk
The risk of osteoporosis in postmenopausal Caucasian women is well known. However, men and women of other races and minority ethnicities may also have a higher osteoporosis fracture risk due to various factors, such as diet, stature, cultural influences, language skills, and economic status.
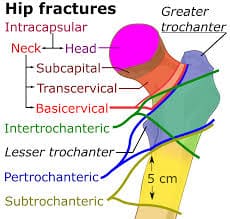
For example, the incidence of hip fractures varies widely around the world based on ethnicity and race. In the United States, the lifetime risk of hip fractures at age 50 is approximately 16 percent in women and 6 percent in men. In comparison, this risk is about 2.5 percent in Chinese women and 2 percent in Chinese men. The highest hip fracture rates are seen in Northern European countries such as Sweden and Norway (could it be because of a lack of exposure to sunlight?). The prevalence of vertebral (spine) fractures varies from 70 percent in White women to 50 percent in African-American women. Also, there is an interplay between sex and ethnicity. Caucasian women experience hip fractures twice as often as men. However, this difference based on sex is negligible among African-Americans and Asians.
Is My Patient at Risk for an Osteoporotic Fracture?
More women experience fractures than the number of women with heart attacks, death from coronary disease, and breast cancer combined. X-ray techs in general and DXA operators in particular should be aware of the above-mentioned factors when they see patients for bone density measurement. In particular, patients with low bone mass (osteopenia) may benefit from advice to improve their bone health and reduce their risk of fractures. Further consultation should be requested if there is suspicion that the patient is at osteoporosis fracture risk despite a a normal DXA result and T-score.
X-ray Continuing Education
Browse our website for a range of online continuing education courses for X-ray techs. Our Radiographic Bone Densitometry course is worth 23 ARRT® category A credits.
Get more information about mri ce credits and x ray continuing education here.