Role of a Radiologic Technologist During Radiologic Crisis

As radiologic technologists, we are uniquely qualified to participate in the medical response to radiologic accidents and radiologic terrorist attacks. Should such incidents occur in our area, our colleagues and the public at large will have the expectation that we will know how to deal with radiation safely since we work with it every day. This article offers information to help you feel comfortable that you can safely help others during such a horrible crisis.
In order to safely work during a radiologic disaster, you need to understand 3 basic things.
-
- Understand what radiation is and know the different types of radioactive materials.
- Know what types of incidents are likely to release those types of materials.
- Know how to deal with patients, decedents, and materials that may be contaminated
Understanding Ionizing Radiation
As radiologic technologists, we possess a deep understanding of ionizing radiation. However, it is always beneficial to keep our knowledge up-to-date. Ionizing radiation might not be a daily conversation topic, but staying informed about its principles and safety measures is crucial for our profession.
Refreshing Your Knowledge
For those looking to refresh their knowledge, our comprehensive course, “Understanding Ionizing Radiation,” provides an excellent opportunity. This course offers 12 ARRT® CE Credits and covers essential aspects of ionizing radiation and its safe handling.
“This course is designed to enhance your understanding and ensure you are well-equipped to manage and utilize radiation effectively in your practice.”
Additional Learning Resources
Moreover, there are valuable resources available for further learning. For instance, the CDC offers some informative videos on the subject. These videos are a great way to visually grasp the fundamentals and advanced concepts of ionizing radiation, making complex information more accessible and easier to understand.
Ensuring Safety and Efficacy
By continually updating our knowledge and skills in this critical area, we ensure the highest standards of safety and efficacy in our radiologic practices. This approach ultimately benefits both our professional development and the well-being of our patients.
Radiological Incidents
Radiological incidents can occur unexpectedly and can be either intentional, such as those caused by acts of terrorism, or unintentional, stemming from accidents or natural disasters. As radiologic technologists, it is crucial to be well-prepared to respond effectively to these emergencies to protect both the public and healthcare personnel.
Intentional Radiological Incidents
Intentional radiological incidents involve the deliberate release of radioactive materials, posing significant challenges:
- Radiological Dispersal Devices (RDDs): Commonly known as “dirty bombs.”
- Malicious Contamination: Deliberate contamination of public spaces with radioactive substances.
“Understanding the nature of these threats and the appropriate response protocols is essential for minimizing harm and ensuring a swift, effective reaction.”
Unintentional Radiological Incidents
Unintentional incidents may result from:
- Industrial Accidents: Accidents during industrial processes involving radioactive materials.
- Transportation Mishaps: Incidents during the transport of radioactive substances.
- Natural Disasters: Earthquakes or other events damaging nuclear facilities.
These incidents can lead to the accidental release of radiation into the environment, requiring immediate action to contain the spread and mitigate exposure risks.
Preparedness and Training
Preparedness for radiological emergencies involves:
- Comprehensive Training: Regular drills to ensure familiarity with emergency procedures.
- Personal Protective Equipment (PPE): Proper use of PPE to protect healthcare providers.
- Decontamination Techniques: Effective methods to decontaminate exposed individuals.
- Management of Exposed Individuals: Protocols for treating those exposed to radiation.
Communication Protocols
Clear understanding of communication protocols is vital:
- Emergency Responders: Efficient communication with emergency teams.
- Public Health Officials: Coordination with public health authorities.
- The Public: Keeping the public informed and safe.
Continuous Education and Resources
Staying informed about the latest guidelines and best practices is essential. Resources such as the CDC’s radiation emergency resources offer valuable information and training materials to help radiologic technologists stay prepared for any radiological emergency.
“Continuous education ensures that we can protect ourselves, our patients, and the community effectively in the event of a radiation emergency.”
Summary
Being well-prepared for radiological incidents, whether intentional or unintentional, is a critical aspect of our role as radiologic technologists. It ensures that we can protect ourselves, our patients, and the community effectively in the event of a radiation emergency.
Improvised Nuclear Device and Nuclear Weapons
Nuclear weapons are highly destructive devices that utilize nuclear reactions, either fission or fusion, to produce immense explosive energy. These weapons can cause catastrophic damage, loss of life, and long-term environmental harm.
Understanding Improvised Nuclear Devices (INDs)
An Improvised Nuclear Device (IND) is a type of nuclear weapon assembled from stolen or illegally obtained nuclear materials. Unlike traditional nuclear weapons developed by nation-states, INDs are typically created by non-state actors, such as terrorist groups, with the intent to cause maximum destruction and chaos. Despite their makeshift nature, INDs can be as devastating as conventional nuclear weapons.
Energy Released by Nuclear Detonation
When an IND or nuclear weapon detonates, it releases four primary forms of energy:
- Blast Wave: The explosion generates a powerful blast wave that can obliterate buildings, infrastructure, and cause significant casualties. The pressure from the blast wave can also result in severe injuries and fatalities to those in its path.
- Intense Heat: The detonation produces an extreme heat wave, capable of causing widespread fires and severe burns to individuals even at considerable distances from the blast site. The thermal radiation can lead to large-scale destruction and secondary fires.
- Light: A nuclear explosion emits a blinding flash of light, which can cause temporary or permanent blindness to anyone who looks directly at it. This intense light contributes to the overall sensory and psychological impact of the explosion.
- Radiation: The explosion releases significant amounts of ionizing radiation, which can penetrate living tissue and cause acute radiation sickness, long-term health issues, and environmental contamination. Exposure to this radiation increases the risk of cancer and other serious health conditions.
“Nuclear explosions also produce fallout, consisting of radioactive particles that contaminate land, water, and the food supply.”
Fallout and Its Implications
Fallout from a nuclear explosion consists of radioactive particles that are propelled into the atmosphere and can travel long distances. This fallout eventually settles back to the ground, contaminating land, water, and the food supply. The radioactive contamination poses severe health risks to all living organisms and complicates recovery and decontamination efforts.
Importance for Healthcare Professionals
For radiologic technologists and other healthcare professionals, understanding the implications of INDs and nuclear weapons is critical. Knowledge of these devices and their effects enables better preparation and response to such incidents, focusing on immediate medical care, long-term health monitoring, and environmental remediation.
Dirty Bomb or Radiological Dispersal Device (RDD)
A dirty bomb, also known as a Radiological Dispersal Device (RDD), combines conventional explosives like dynamite with radioactive materials in the form of powder or pellets. Unlike a nuclear weapon, a dirty bomb does not initiate a nuclear reaction and cannot create an atomic blast. However, it poses significant dangers through the dispersion of radioactive materials.
How a Dirty Bomb Works
When the explosives in a dirty bomb detonate, the force of the blast scatters the radioactive materials into the surrounding environment. The dispersal can contaminate a wide area, depending on factors such as wind conditions and the type of radioactive material used. The primary objective of an RDD is not to cause mass destruction through the explosion itself but to spread radioactive contamination, thereby creating fear, panic, and disruption.
Immediate Impact
The immediate impact of a dirty bomb includes:
- Blast Damage: Injuries, fatalities, and structural damage typical of any explosive device.
- Radioactive Contamination: The spread of radioactive material poses long-term health risks.
“Radiation exposure can lead to acute radiation sickness, increased cancer risk, and other serious health issues over time.”
Emergency Response Steps
Responding to a dirty bomb involves several critical steps:
- Treating Blast Injuries: Immediate medical attention for injuries caused by the explosion.
- Preventing Further Exposure: Evacuating the affected area and decontaminating exposed individuals.
- Using Protective Gear: Ensuring the safety of first responders and medical personnel.
- Environmental Cleanup: Managing contamination and protecting public health.
- Long-Term Monitoring: Continuous health monitoring for those exposed to radiation.
Importance for Healthcare Professionals
Understanding the mechanics and implications of a dirty bomb is crucial for radiologic technologists and other healthcare professionals. Being prepared to respond effectively to such incidents involves:
- Staying Informed: Keeping up with radiation safety protocols and emergency procedures.
- Emergency Procedures: Knowing the steps to take during and after an incident.
- Decontamination Techniques: Proper methods for decontaminating exposed individuals.
Continuous Education and Training
Continuous education and training are key to ensuring readiness for these complex emergencies. Resources like the CDC’s radiation emergency resources offer valuable information and training materials.
Radiological Exposure Device (RED)
A Radiological Exposure Device (RED), also known as a hidden sealed source, is a malicious device containing radioactive material designed to expose individuals to radiation without their knowledge. Unlike explosive devices, REDs do not rely on a blast to disperse radioactive material. Instead, they are covertly placed in locations where people will unknowingly come into proximity with the radiation source.
How REDs Work
REDs are typically made from radioactive materials sealed within a container that shields them from detection. These devices can be strategically hidden in:
- Public places
- Workplaces
- High-traffic areas
The primary intent of an RED is to cause radiation sickness, long-term health issues, and widespread fear without immediate, obvious signs of an attack.
Effects of Exposure
The effects of exposure to an RED depend on several factors:
- Type and amount of radioactive material: The specific radioactive material used.
- Duration of exposure: How long individuals are exposed to the radiation.
- Proximity to the device: How close individuals are to the radiation source.
“Acute exposure can lead to radiation sickness, characterized by symptoms such as nausea, vomiting, fatigue, and skin burns. Long-term exposure increases the risk of cancer and other serious health conditions.”
Detection and Response
Detecting and responding to REDs pose significant challenges:
- Detection: Identifying the presence of REDs requires specialized equipment such as Geiger counters and dosimeters.
- Immediate Action: Once an RED is identified, immediate steps must be taken to minimize exposure, including evacuating the area and securing the device.
- Decontamination: Conduct a thorough decontamination process to ensure all traces of radioactive material are safely removed.
- Public Communication: Inform and reassure those who may have been exposed.
Importance for Healthcare Professionals
For radiologic technologists and other healthcare professionals, understanding the nature and risks associated with REDs is crucial. Preparedness includes:
- Training in the use of radiation detection equipment
- Knowing protocols for handling radiation emergencies
- Staying informed about the latest safety guidelines and response strategies
Nuclear Power Plant Accident
An accident at a nuclear power plant can release significant amounts of radiation, posing serious health and environmental risks. Such incidents can result from equipment failure, human error, natural disasters, or external attacks. The consequences can be far-reaching, affecting both the immediate vicinity and distant regions depending on weather conditions and the nature of the release.
Safety and Security Measures
Nuclear power plants are equipped with numerous safety and security measures to prevent accidents and minimize impacts:
- Multiple layers of physical barriers
- Automated shutdown mechanisms
- Redundant cooling systems to manage reactor temperature and prevent overheating
These facilities are closely regulated by the Nuclear Regulatory Commission (NRC), which enforces stringent standards for construction, operation, and emergency response.
“Safety systems at nuclear power plants include multiple layers of physical barriers, automated shutdown mechanisms, and redundant cooling systems.”
Immediate Response to an Accident
Despite these precautions, the possibility of an accident cannot be entirely eliminated. In the event of a radiation release, immediate actions are taken to protect public health and safety:
- Activating emergency response plans
- Evacuating affected areas
- Providing clear communication to the public about protective measures
Long-Term Response
Long-term responses involve:
- Monitoring radiation levels
- Decontaminating affected areas
- Assessing the health impacts on the population
Role of Healthcare Professionals
The role of radiologic technologists and healthcare professionals in such scenarios is crucial. Key responsibilities include:
- Understanding the potential health effects of radiation exposure
- Using protective equipment effectively
- Assisting in the medical management of exposed individuals
Continuous Education and Preparedness
Continuous education on radiation safety and emergency procedures, as well as staying informed about advancements in nuclear safety technology, are vital for maintaining readiness. For more information, visit the CDC’s radiation emergency resources.
For additional resources and continuing education opportunities in radiography, explore CE4RT.
This video discusses the difference between nuclear and radiologic incidents.
video credit : ORAU IMA
Radiologic Incident Response
Radiation cannot be detected by the human senses, making it a particularly insidious hazard. Specialized equipment is required to conduct a radiological survey and confirm the presence of radiation. In the event of a terrorist attack involving radioactive materials, it is crucial to assess both patient exposure and contamination accurately.
Understanding Radiation Exposure
Exposure occurs when a person is near a radiation source. Key points about radiation exposure include:
- Individuals exposed to significant levels of radiation can suffer from radiation sickness, characterized by symptoms such as nausea, vomiting, and fatigue.
- Exposure alone does not make a person radioactive. For example, after a chest X-ray, a person does not become radioactive or pose any risk to others.
Contamination
Contamination involves the deposition of radioactive particles on surfaces, skin, or clothing. It can be classified as:
- External Contamination: Managed by removing and properly disposing of contaminated clothing and thoroughly washing the skin.
- Internal Contamination: Occurs when radioactive particles are inhaled, ingested, or enter the body through open wounds, posing more complex health risks as the particles can remain in the body and irradiate tissues over time.
“Exposure alone does not make a person radioactive. Understanding this distinction is crucial for effective radiologic incident response.”
Decontamination Process
In the wake of a radiological incident, contaminated patients should be decontaminated promptly to prevent further radiation exposure and spread of radioactive materials. The process includes:
- Removing contaminated clothing
- Rinsing exposed skin with water
- Using specialized decontamination solutions when necessary
It is important to perform decontamination swiftly but not delay the administration of critical care.
Treatment for Exposed Patients
Patients exposed to radiation but not carrying radioactive contaminants do not require decontamination. They should be:
- Monitored for symptoms of radiation sickness
- Treated based on their level of exposure
Radiologic technologists must distinguish between exposure and contamination to apply the appropriate response measures effectively.
Continuous Education and Training
Continuous education and training on radiation safety and incident response protocols are vital for radiologic technologists. Staying updated with the latest guidelines and best practices ensures readiness to handle radiological emergencies efficiently and safeguard public health.
Medical Management Principles
When managing patients involved in radiological incidents, the primary principle is to ensure that the treatment of life-threatening injuries is not delayed by contamination concerns. Immediate medical care must take precedence to stabilize the patient, even if radiological decontamination is necessary.
Prioritizing Immediate Medical Care
Key points include:
- Life-Saving Treatment First: Stabilize the patient before addressing contamination concerns.
- Standard Precautions: Use protective gear, such as gloves and gowns, to provide adequate protection against potential exposure.
“Immediate medical care must take precedence to stabilize the patient, even if radiological decontamination is necessary.”
Understanding Health Risks to Providers
The levels of radioactivity typically associated with contaminated patients are unlikely to pose a significant health risk to healthcare providers. Standard precautions generally provide adequate protection. However, providers should always follow established safety protocols to minimize any risks.
Handling Severe Contamination
In rare cases, patients may present with embedded radioactive fragments or large amounts of external contamination. These situations require expedited decontamination:
- Swift Removal: Remove contaminated clothing immediately.
- Thorough Washing: Wash the skin thoroughly to remove contaminants.
- Specialized Equipment: Use specialized decontamination solutions as necessary.
Involving Radiation Professionals
Including in-house radiation professionals on the response team is crucial for effective management of radiological incidents. Their expertise ensures that both patients and healthcare providers are protected, and the response is conducted efficiently and safely. These experts provide guidance on:
- Radiation safety
- Decontamination procedures
- Use of detection equipment
Summary of Key Principles
The key medical management principles for radiological incidents include:
- Prioritization of life-saving treatment
- Low risk of significant health hazards to care providers from contaminated patients
- Prompt decontamination in specific cases
- Inclusion of radiation professionals in the response team
Continuous training and adherence to these principles are essential for optimal outcomes in radiological emergencies.
STAFF PROTECTION GUIDELINES
Establish an ad hoc triage area.
-
- Base the location on your hospital’s disaster plan and the anticipated number of casualties.
- Establish a contaminated area and clean area separated by a buffer zone.
- Remove your contaminated outer garments when leaving the contaminated area.
- Have your body surveyed with a radiation meter when exiting a contaminated area.
Use standard precautions to protect staff.
-
- Follow standard guidelines for protection from microbiological contamination.
- Surgical masks should be adequate.
- N95 masks, if available, are recommended.
- Survey hands and clothing at frequent intervals with a radiation meter.
- Due to fetal sensitivity to radiation, assign pregnant staff to other duties.
DECONTAMINATION GUIDELINES
Survey the patient with a radiation meter.
-
- Perform surveys using consistent technique and trained personnel.
- Note exceptionally large amounts of surface or imbedded radioactive material.
- Handle radioactive objects with forceps and store in lead containers.
- Record location and level of any contamination found.
Remove patient clothing.
Carefully cut and roll clothing away from the face to contain the contamination.
Double-bag clothing using radioactive hazardous waste guidelines, label, and save as evidence.
Repeat patient survey and record levels.
Cleanse contaminated areas.
-
- Wash wounds first with saline or water.
- If facial contamination is present, flush eyes, nose, and ears, and rinse mouth.
- Gently cleanse intact skin with soap and water, starting outside the contaminated area and washing inward.
- Do not irritate or abrade the skin.
- Resurvey and note levels.
- Repeat washing until survey indicates radiation level is no more than twice background or the level remains unchanged.
- Cover wounds with waterproof dressing.
- Dispose of waste water through normal channels.
- For mass casualties, consider establishing separate shower areas for ambulatory and non-ambulatory patients.
RADIATION-RELATED ILLNESS/INJURY
Acute radiation syndrome (ARS)
-
- ARS is caused by high doses of radiation being rapidly delivered to large portions of the body. The most probable terrorist events, such as the use of a dirty bomb, will likely generate low levels of radiation exposure. If ARS cases are seen, small casualty numbers are likely.
- Time of exposure, distance from radioactive source, and duration of exposure should be noted.
- Patients can present individually if exposed to radioactive sources hidden in the community.
- Symptoms can be immediate or delayed, mild or severe, based on radiation dose.
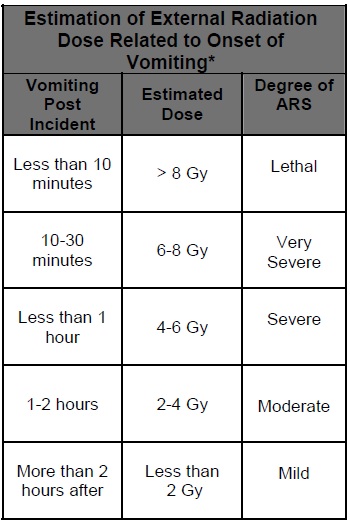
- Nausea, vomiting may occur minutes to days after exposure. Time of onset of vomiting is a major factor in diagnosis and dose estimation (See Table 1).
- Early onset of vomiting followed by symptoms of bone marrow suppression, gastrointestinal destruction, and/or cardiovascular/central nervous system effects is indicative of acute illness.
- Depending on the stage of illness, a patient may be asymptomatic.
Diagnosis and treatment
-
- Perform sequential CBCs with differential to assess progressive declines in lymphocyte levels (See Andrews Lymphocyte Nomogram).
- Monitor for fluid and electrolyte balance and evidence of hemodynamic instability.
- Treat symptomatically with focus on prevention of infection, including antibiotics.
- Consider cytokines, e.g. Neupogen®, and hematopoietic growth factors.
- Perform surgical interventions within the first 48 hours or delay until after hematopoietic recovery.
- Consider use of biodosimetry dose assessment software from www.afrri.usuhs.mil.
Cutaneous radiation injury (CRI)
-
- CRI is acute radiation injury to the skin.
- Skin damage can manifest within hours, days, or weeks after radiation exposure.
- Transient itching, tingling, erythema, or edema may be seen within hours or days after exposure, and is usually followed by a latent period.
- Lesions may not be seen for weeks to months post exposure, but then can be debilitating or even life-threatening.
- Delayed occurrence of lesions is a differentiating factor from thermal burns.
- Note time of occurrence of signs and symptoms and progressive changes in appearance.
- Treat localized injuries symptomatically, focusing on pain and infection control.
Internal contamination
-
- Internal contamination should be considered if persistently high survey readings are noted following decontamination. Internal contamination generally does not cause early symptoms.
- Nose or mouth contamination may indicate inhalation or ingestion.
- Assessment may include analysis of urine, blood, and fecal samples or whole body counts. Consult with radiation experts.
- Radiation experts may recommend early administration of radionuclide-specific decorporation agents such as Prussian Blue, DTPA, or Bicarbonate.
- Gastric lavage, antacids, and cathartics assist in clearing ingested contaminants.
Psychosocial issues
-
- In urban areas, hundreds to thousands may seek care. The majority will self-refer to the nearest hospital. Many will need decontamination. Many may seek radiological screening, but will not be contaminated. Many will simply seek reassurance.
- Psychogenic illness symptoms, such as nausea or vomiting, may manifest.
- Vomiting due to radiation exposure is usually recurrent rather than episodic.
- Include mental health professionals on the response team.
- Have radiation exposure fact sheets available for patients and families.
- Pregnant patients require special counseling.
- Separate areas for radiation screening and counseling could be needed for patients with minimal risk of exposure or injury.
MANAGEMENT OF DECEASED
If exposed to a lethal dose of radiation without contamination, a patient is not radioactive and no special precautions are needed.
Special precautions may be necessary for contaminated deceased.
Video Reference
This video by the CDC is a good overview and outlines the basics of clinicians response to radiological incidents.
How to use a geiger counter to screen patients.
video credit : Kids With No Money
More information is available from the CDC at https://emergency.cdc.gov/radiation/resourcelibrary/all.asp