Skull Fracture
The skull is made up of numerous flat bones that are connected by cranial sutures. Each flat bone has a thick outer table, a spongy diploe, and a narrower interior table. A thick, fibrous, adhesive dura mater lines the inner table. A narrow subdural gap exists between the dura’s inner surface and the thin arachnoid mater covering the brain.
A skull fracture is a break in the bone of the skull that usually develops as a consequence of direct trauma. Localized impact deforms the skull, which may cause harm to the cranial contents even if the skull does not fracture. Skull fractures are prevalent in both closed traumatic brain injury and penetrating traumatic brain injury. Their significance stems from the fact that they are related to a range of soft tissue injuries depending on their location.
A head injury and a skull fracture are not the same; rather, a skull fracture can be considered as part of a head injury. First, what exactly is a head injury?
A head injury is caused by damage to the scalp, skull, or brain. Head injuries are characterized as either closed (no cut or laceration to the skin) or penetrating (the skin and/or bone of the skull is fractured). Traumatic brain injuries range in severity from minor (referred to as mild traumatic brain injury) to severe (referred to as severe traumatic brain injury).
The symptoms of a head injury may appear shortly after the impact or they may appear gradually over several hours or days. The following are examples of specific types and symptoms of brain injuries:
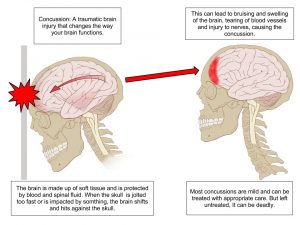
A concussion is sometimes known as a mild traumatic brain injury. This includes brain injuries produced by a blow to the head or body, a fall, or another type of trauma that rattles or shakes the brain inside the skull. Concussion victims may not always display symptoms that are visible to others. Concussions and mild head injuries can cause the following symptoms:
awareness loss ranging from a few seconds to a few minutes
consternation; memory and/or focus issues
dizziness
headache
Amnesia; memory loss of events occurring prior to or soon following the injury
vomiting and nausea
A changed state of awareness, such as drowsiness or difficulty waking up
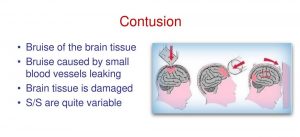
A bruise of the brain tissue is frequently linked with swelling (edema) and a rise in intracranial pressure (ICP). Dilated pupils are one of the symptoms of increased pressure within the brain and the skull. Other than that, the blood pressure could be too high, the patient may have a low pulse rate, irregular breathing, etc.
A fracture is a break in the skull with or without a skin laceration. Tenderness is one of the symptoms of a skull fracture. Swelling, skull distortion, bruising around the eyes or behind the ear, and clear fluid pouring from the nose or ear are all symptoms of a skull fracture.
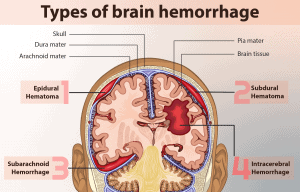
Bleeding in the brain, commonly known as a hemorrhage, is a potentially fatal disease that, in many situations, needs immediate care from a neurosurgeon. When a blood artery in the brain ruptures, it causes bleeding into surrounding tissue, edema, and increased intracranial pressure. Blood can also accumulate and form a clot, known as a hematoma. Clotting develops between the skull’s interior and the brain’s outer, robust membranous covering in an epidural hematoma (called the dura mater). A subdural hematoma is a collection of blood beneath the dura mater. The following symptoms of brain hemorrhage may start quickly or progressively worsen: sudden severe headache, convulsions nausea, or recurrent vomiting and lethargy, as well as loss of consciousness due to arm or leg weakness.
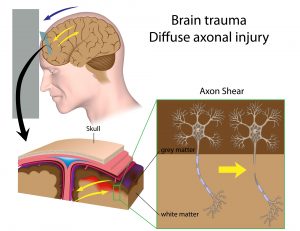
Shear damage (also known as diffuse axonal injury) occurs when the brain collides violently with the inside of the skull. Nerve fibers that extend from the central body of a nerve cell are stretched or ripped, causing irreversible damage to brain cells and other issues within the nervous system. A shear injury’s principal symptom is a protracted loss of consciousness. Patients who display signs of brain injury should seek medical assistance immediately.
Head injuries are treated differently depending on the type of damage and the patient’s health. A physician may undertake a physical and neurologic exam, along with imaging studies to determine the severity of a head injury.
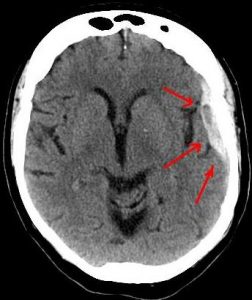
CT scan of the head : CT scan of the head is performed. CT scanning combines specialized X-ray equipment with advanced computers to generate numerous images or photos of the head and brain. Doctors use CT scans of the head to identify bleeding, edema, brain damage, and skull fractures. More information regarding CT may be found on the Safety page.
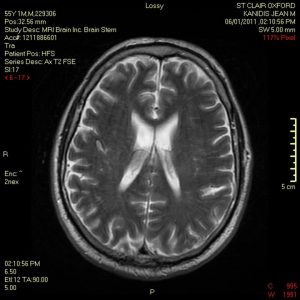
MRI of the brain: Magnetic Resonance Imaging (MRI) creates comprehensive images of organs, soft tissues, bone, and almost all other internal body components by using a high magnetic field, radiofrequency pulses, and a computer. In certain cases, clinicians will employ an MRI of the brain, including advanced MR scanning techniques such as diffusion-weighted imaging, diffusion tensor imaging, and MR spectroscopy, to help diagnose brain injuries that do not show up on a standard MR scan.
X-ray of the head: An X-ray is a procedure that includes exposing a portion of the body to a low dosage of ionizing radiation in order to obtain images of the inside of the body. Doctors occasionally use an X-ray of the head to discover and assess skull fractures. However, such an exam is rarely used nowadays because it cannot check the brain at all. A CT scan can show most skull fractures more clearly than a head X-ray.

Furthermore, clinicians clearly understand that it is more necessary to establish underlying brain damage in order to decide the right therapy for the patient. CT and, if necessary, MRI are the primary imaging methods for this purpose.
Skull fractures, on the other hand, can be generally classified as follows:
anatomically
base of skull
skull vault (calvaria)
associated with an overlying wound
open (compound)
closed
degree of displacement
undisplaced
depressed (5 to 10 mm)
number of fracture lines/fragments
linear
comminuted
Fractures of the skull, like fractures of any other bone, occur when biomechanical forces surpass the tolerance of the bone. The fracture pattern is determined by the position, direction, and kinematic aspects of the hit, along with intrinsic skull traits.
Radiographic features
Plain radiographs
Plain radiographs have a limited purpose, and are being phased out in favor of CT scans. They are no longer suggested for assessing head injuries unless they are part of a skeletal assessment for a suspected non-accidental child injury.
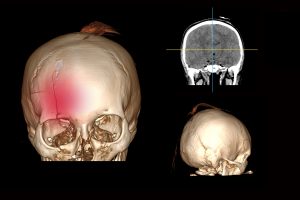
CT scan
A CT scan of the brain is the best way to visualize skull fractures. CT is not only sensitive to the diagnosis of fractures, but it may also describe their extent and assist in surgical planning. It is also collected at the same time that the brain is scanned.
A volumetric CT of the skull with tiny (1 mm) voxels that can be reconstructed in several planes should be obtained. If nondisplaced fractures are to be viewed, a bone algorithm must be utilized.
Fractures occur as discontinuities in the bone, and they may or may not be displaced. They must be recognized from normal sutures, which lack the corticated borders found in fractures. If the fracture affects a paranasal sinus, middle ear, or mastoid air cell, it will almost always contain some blood, which is a useful signal of the presence of an underlying fracture.
A thorough search for nearby soft tissue injuries should be performed when a fracture is found. Soft tissue injuries include the following:
Vascular:
arterial dissection, occlusion, or rupture
arterial extradural hemorrhage
arteriovenous fistula (e.g., direct carotid-cavernous fistula)
Dural venous sinus injury
venous extradural hemorrhage
Dural venous sinus thrombosis
extension through cranial nerve foramina or canals with neural damage
underlying cerebral hemorrhagic contusions
Dural tears leading to CSF leak and intracranial hypotension
MRI
MRI is insensitive to fractures, and it is frequently startling how difficult it is to image fractures even when they are obvious and well-documented on a CT.
Skull fractures that are closed and nondisplaced seldom require direct management, with therapy focusing on any related damage (e.g., extradural hematoma). Depressed fractures, on the other hand, frequently necessitate surgical intervention for cosmesis and a decrease in the frequency of post-traumatic epilepsy. Debridement is frequently required after an open (complex) fracture to limit the risk of infection.
Sources:
https://radiopaedia.org/articles/skull-fractures
https://www.radiologyinfo.org/en/info/headinjury
Get more information about radiologic technology continuing education and arrt ce credits online here.
