Reducing Radiation Exposure in Digital Imaging

Digital imaging techniques provide important information to healthcare professionals. But, exposure to ionizing radiation can be harmful to patients. In digital fluoroscopy, an increase in the number of images per exam reveals greater diagnostic information but is associated with an increased dose. Similarly, magnification improves spatial resolution and image quality but may lead to an increase in skin dose. High-dose mode is associated with an improvement in image quality but is associated with a high radiation dose to the patient. What are some of the methods of reducing radiation exposure? What can X-ray techs do to follow the ALARA principle and ensure the safety of their patients?
Techniques such as virtual collimation and pulsed fluoroscopy decrease patient dose with either no effect or only a slight degradation in image quality. There are several ways of reducing radiation exposure of patients and minimizing risk without compromising the health benefits of a radiological procedure. A high benefit/risk ratio for radiological procedures is to a large extent dependent on correct procedure selection, proper technique, and quality control. For instance, studies have shown that the use of automatic exposure control (AEC) can significantly reduce patient dose. In digital imaging, a lack of collimation or discarding apparently non-useful images can lead to a need for repeat imaging and increased patient exposure.
Factors Affecting Patient Radiation Dose
The radiation dose delivered to a patient by an imaging examination is affected by several factors, including patient-specific factors such as age and body habitus, the imaging modality used and technical factors selected, and the skill and experience of the technologist. One method of reducing radiation exposure in diagnostic radiology is by justifying the examination, avoiding repetitions, and maintaining complete medical records. Up-to-date clinical information and compilation of a past imaging record ensures that useless tests are not performed. The outcome of the proposed examination, whether positive or negative, should impact the patient’s management and/or strengthen the treating physician’s confidence in the diagnosis. It is also important to consider the possibility of obtaining similar information from non-radiating modalities, such as ultrasound and MRI, if cost and logistics are not prohibitive.
High-Dose Procedures
Certain high-dose diagnostic examinations require careful consideration. The higher the dose associated with a procedure, the greater the risk of radiation effects. It stands to reason then that such procedures should be carefully justified before they are performed. Fluoroscopically-guided interventions are a subset of potentially high-dose procedures which can cause complications called tissue reactions (skin erythema, hair loss), although such injuries are rare. Computed tomography images, especially multi-slice or spiral scans, allow useful information to be obtained easily. The temptation, therefore, is to frequently monitor patients with CT examinations. However, this temptation should be tempered by the fact that these examinations deliver high doses of ionizing radiation to the patient. Therefore, limiting the number of studies obtained is an important method of reducing radiation exposure.
Procedure Optimization
Optimization of the procedure is a powerful tool for reducing radiation exposure of patients undergoing diagnostic examinations. The radiologist, radiologic technologist, and medical physicist must work together to ensure that every examination provides the necessary diagnostic information and satisfactory image quality at a dose which is as low as reasonably possible and keeping in mind financial and social factors.
Ruling Out Pregnancy
Before beginning a digital radiographic examination, the radiologic technologist must question female patients with childbearing potential about the possibility of pregnancy. Department protocols vary, but this typically involves carefully reviewing the patient’s medical history, asking leading questions, and making note of physical signs. Professionalism and tact are necessary during this communication to put the patient at ease. The need for a pregnancy test is determined by the referring physician and/or radiologist in line with department protocols. The physicians also decide whether alternative non-radiating imaging modalities should be considered to reduce radiation exposure. It is best practice to screen females of childbearing age for possible pregnancy before radiographic examinations.
The Radiologic Technologist’s Role in Reducing Radiation Exposure
The radiographer is the individual who operates the X-ray equipment and controls the primary beam which delivers radiation to the patient. A number of adjustable technical factors can help optimize the patient’s radiation exposure. X-ray tube voltage and current are two of the most important factors that influence the critical balance between the radiation dose delivered and the image quality achieved. An appropriate balance between the two is a vital part of procedure optimization. It is desirable to use the highest kV and lowest mA compatible with the necessary image quality in order to minimize the dose. Technique charts are available near each X-ray control panel. These charts specify the parameters that should be used for manual exposures of body parts of varying thickness. In systems with automatic exposure control, the technique chart specifies the settings on the control panel that should be used for each projection. It is a good radiological practice to update technique charts from time to time.
Tube Voltage and Tube Current
Subject contrast in a radiographic image can be altered by manipulating exposure factors, i.e., tube voltage and tube current. The X-ray beam contains a spectrum of energies. The tube voltage (kV) determines the maximum energy or penetrating power of the beam. High-energy X-rays penetrate the patient’s body and exit it to form the image. X-rays with low energy enter the patient’s body and add to radiation dose without contributing to image formation. Low kV also produces more scatter radiation. The patient’s radiation dose is higher when the beam contains more low-energy X-rays (low kV). A 120 kV tube produces more high-energy X-rays and delivers a lower radiation dose than a 50 kV tube. A high kV is thus desirable. In other words, one way of reducing radiation exposure is increasing the tube voltage. However, the tube voltage cannot be increased indefinitely because it results in a loss in image contrast. Dense structures, such as bone, are visualized well with high tube voltage, but soft tissue visualization requires the use of lower kV.
Tube current (mA) determines the number of X-rays produced per unit time. A higher tube current is associated with less image noise, but it exposes the patient to a larger radiation dose. For example, compared to a tube current of 10 mA, a tube current of 800 mA will produce less noise in the image but will deliver 80 times more radiation to the patient. A low mA is thus desirable. The right balance between kV and mA is necessary for adequate image quality with the least possible dose. For example, an AP knee radiograph at 55 kV and 9 mA may not produce a clinically useful image of the dense bones in the area of interest. On the other hand, when exposure factors are changed to 70 kV and 3 mA, there is better penetration of the dense knee structures, and importantly, the patient receives a lower dose. It should be noted that to adequately penetrate a plaster of Paris cast which is quite dense, both exposure factors (kV and mA) often need to be increased.
Exposure Technique Charts
Exposure technique charts provide radiographers with preprogrammed settings for the positions used and procedures routinely performed in a radiography unit. These settings are the exposure recommendations for adult patients of various sizes (small, medium, large) and include a combination of manual exposure and AEC settings. The radiographer should not blindly follow a technique chart, however. Instead, the appropriateness of the exposure technique should be assessed for the specific radiographic study and patient’s medical condition as well as any unusual circumstances. It is worth remembering that exposure technique charts are developed keeping in mind a typical patient. The time and effort that goes into developing exposure technique charts pays off in terms of reduced technical errors and greater consistency. Exposure technique charts reduce patient dose by ensuring accurate and consistent exposure of the image receptor. These charts help radiographers follow department standards with regards to variables such as kVp, mAs, source-to-image receptor distance, use of anti-scatter grid, focal spot size, and AEC detector selection. It is best practice for radiographers to use standardized exposure technique charts and for the department to continuously improve these charts.
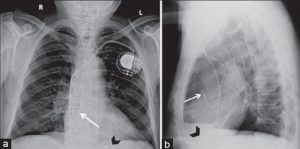
Lead Markers
Lead markers indicating the anatomical side should be placed on the image receptor during image acquisition. It is not acceptable to annotate anatomic side during image postprocessing. The failure to use anatomical side lead markers is a legal issue. It is best practice to consistently use lead markers to indicate the anatomic side at the time of X-ray exposure.
Portable Radiography and CT Examinations
With portable X-ray equipment, technologists should take care that the source-to-skin distance is at least 30 cm. With fixed equipment, the distance from the source to the patient should be at least 45 cm. In general, the source-to-skin distance should be maximized and the patient-to-detector distance should be minimized. Portable X-ray equipment is operated with a high instantaneous electrical power supply because inadequate power produces poor quality images. Battery-operated portable units should be operated on full charge to avoid retakes due to poor image quality. Since fluoroscopic procedures are associated with high doses, the fluoroscopy time should be minimized to reduce radiation exposure. A timer is used to measure the elapsed exposure time and an audible alarm sounds every 5 minutes as a reminder to the radiographer. Fluoroscopic imaging devices have dose-saving features such as pulse mode and last image hold (which allows the radiologist to view the last fluoroscopic image captured). The least number of slices should be used during CT examinations since a higher number of slices is associated with a larger patient dose.
Reasons for Repeat Exams
The advent of digital imaging technology has seen an overall reduction in the number of repeat examinations obtained because of the wide exposure range of these systems. However, the number one reason for repeat examinations has shifted from exposure errors in film-screen systems to patient positioning errors in digital systems. Therefore, accurate patient positioning is critical to avoid repeats and keep radiation dose in check. Poor collimation and inaccurate positioning of the area of interest relative to the image receptor can result in digital images that are not diagnostically useful. Radiographers should position the patient according to department guidelines and national standards to avoid repeat examinations. To this end, immobilization with plastic devices, sandbags, and sponges is particularly important in pediatric patients. It is best practice to correctly position the patient (using immobilization devices if necessary) to avoid repeat exposures.
Exposure Indicator and Deviation Index
When it comes to radiation safety, it does not help matters that equipment manufacturers often use different terminology for similar features. The use of consistent terminology for exposure indicator (EI) is one effort to this end.
As noted, the nomenclature for exposure indicator is variable amongst manufacturers of digital radiography equipment, and this can be confusing for radiologic technologists. To address this issue, the IEC has worked with other organizations to develop and implement a standard and consistent EI terminology that is applicable to all types of image receptors. Radiographers should also be aware of the deviation index (DI) which is a measure of the difference between the actual and target exposure, thereby indicating a need for corrective action and serving as a feedback to the technologist. It is best practice for radiographers to be familiar with the exposure indicator (EI) and deviation index (DI) for the equipment they use and to become familiar with new standardized EI terminology.
Radiographers must understand the exposure factors that affect the EI value and its limitations. One limitation of the exposure indicator is that the value will be inaccurate if the exposure field borders are not correctly recognized. Also, as mentioned, different manufacturers determine EI by analyzing different regions of the image. The wide dynamic range of digital radiography equipment, poor collimation, lack of proper patient positioning, and an unusual body habitus may also affect the EI. Therefore, an acceptable EI is not verification of proper exposure technique. It is best practice for radiographers to use the exposure indicator (EI) to assess adequate exposure of the image receptor. It is best practice to evaluate EI in combination with image quality to ensure the digital image is of an acceptable standard. It is best practice to for the technologist to remember that the EI has limitations and careful consideration should be given to the need for repeat imaging.
ARRT® Continuing Education
We offer a range of online courses for X-ray techs to complete their biannual continuing education requirements. Our e-courses and open-book post-tests are an easy and convenient way to earn category A credits recognized by the ARRT® and other registries. We offer specific courses for mammographers and fluoroscopy techs. We also have bundles of courses for California CE, Florida X-ray CE, and Texas CE for X-ray techs.
Visit here to know more about ionizing radiation and protection.